For women in the United States today, the choices around birth control are both more numerous
and more complex than ever. While nearly all reproductive-age women use some form of contraception at some point.
Recent years have brought new questions, shifting policies and important developments that shape how we access and experience birth control.
From the explosion of telehealth and online birth control services, to political debates and
innovations in technology, the landscape is rapidly evolving. Yet, for many women, finding clear,
reliable information and a method that fits their unique health needs and lifestyle can still be a real challenge.
Consider the statistics: nearly two-thirds of American women aged 15–49 report using a birth
control method today, and almost all women who have had sex will use contraception at some
point. However, barriers remain.
Cost, misinformation, side effects, and changes in state laws all impact our contraceptive choices
and access. Recent federal policies, such as the Affordable Care Act and the proposed Access to
Birth Control Act, have made great strides in expanding coverage, but millions still face difficulties
ranging from insurance hurdles to pharmacy denials.
Meanwhile, the development of both hormonal and non-hormonal methods—tailored to address
users’ health conditions, lifestyles, and even personal preferences—offers more options than
ever, yet can also create confusion. So, what is birth control really, and how do you choose among
the myriad pills, patches, implants, shots and more?
What are the latest trends for 2025 and 2026 in the U.S. market, how do new laws affect access
and what should you know about side effects, cost, and effectiveness?
In this guide, we’ll break down the most common types of birth control (including pills, implants,
patches, and shots), discuss side effects, debunk myths, and answer pressing questions about
getting pregnant on birth control, stopping your periods, and getting your contraceptives online.
We’ll also compare methods, offer U.S.-centric advice, and provide the links and resources you
need to make an empowered decision for your reproductive health.
What Is Birth Control?
Birth control—also called “contraception”—is any method, medicine, or device used to prevent
pregnancy. It works in a variety of ways: by stopping ovulation, thickening cervical mucus to
block sperm, altering the uterine lining to prevent implantation, or physically blocking sperm from
reaching the egg.
Methods are usually classified as hormonal (such as pills, patches, implants, and injections) or
non-hormonal (like copper IUDs, condoms, or fertility-based approaches). Birth control is about more than just preventing pregnancy.
Many women use these methods for other health benefits, including regulating menstrual cycles, reducing period pain, treating conditions like endometriosis or polycystic ovarian syndrome (PCOS), and even improving acne. In short, birth control is a tool for reproductive autonomy, menstrual management, and personal well-being.
Facts
Health services are available for young people to help them prevent unintended pregnancy. It is important that parents know about these services, too.
Did you know?
Over the past decade, the percent of high school-aged adolescents having sex has declined. However, according to Wisconsin Department of Public Instruction in 2023, 31.6% of high school students have had sex.
Where can I get more information about birth control?
Many safe and effective birth control methods are available for adolescents who are, or are considering becoming, sexually active.
They can choose the method that works best for them. Details on the range of birth control methods are available on CDC’s website.
Choosing the right birth control method
Information from parents and health care providers can help adolescents decide which birth control method is right for them.
Key Birth Control Terms
● Birth control pills: Oral contraceptives taken daily.
● Implant: A small rod inserted in the arm that releases progestin.
● Patch: A transdermal patch worn on the skin that releases hormones.
● Shot: An injectable form of progestin received every three months.
● Tablets/Minipills: Refers to both combination (estrogen and progestin) and
progestin-only oral contraceptives.
● Emergency contraception: Pills or devices taken after unprotected sex.
Types of Birth Control: Pills, Tablets, Patch, Implant, Shot, and More
Birth Control Pills Overview
Birth control pills are among the most popular contraceptive methods in the U.S. They come in
two main types: combination pills (containing estrogen and progestin) and progestin-only pills
(also called minipills).
How they work
Pills typically prevent ovulation, thicken cervical mucus, and thin the lining of the uterus. Combination pills are most common, but progestin-only pills are favored for women who cannot take estrogen—such as those at higher risk of blood clots, or who are breastfeeding.
Usage
Pills must be taken daily at the same time for maximum effectiveness. Forgetting doses
increases the chance of pregnancy.
Effectiveness: With perfect use, pills are over 99% effective; with typical use, efficacy drops to
around 91–93% due to missed pills.
Popular birth control pills brand names:
Some common brands in the U.S. include:
● Combination: Alesse, Aviane, Sprintec, Junel FE, Yaz, Yasmin, Lo Loestrin Fe, Ortho-Cyclen,
Microgestin, Levora, Tri-Sprintec, Beyaz, Estarylla
● Progestin-only: Slynd, Camila, Nora-BE, Errin Birth control tablets refer to these oral contraceptive options, including both combination and minipill types.
Side Effects:
● The most common side effects include nausea, headaches, breast tenderness, irregular
bleeding, mood changes, and occasional weight changes (mainly due to fluid retention,
not fat gain).
● Serious risks are rare but include blood clots, stroke, and heart attack—particularly in
women over 35 who smoke.
Non-contraceptive benefits:
● Reduced menstrual cramps and lighter periods
● Lower risk of ovarian and endometrial cancers
● Improvement in acne and hormonal imbalances
● Management of PCOS and endometriosis symptoms.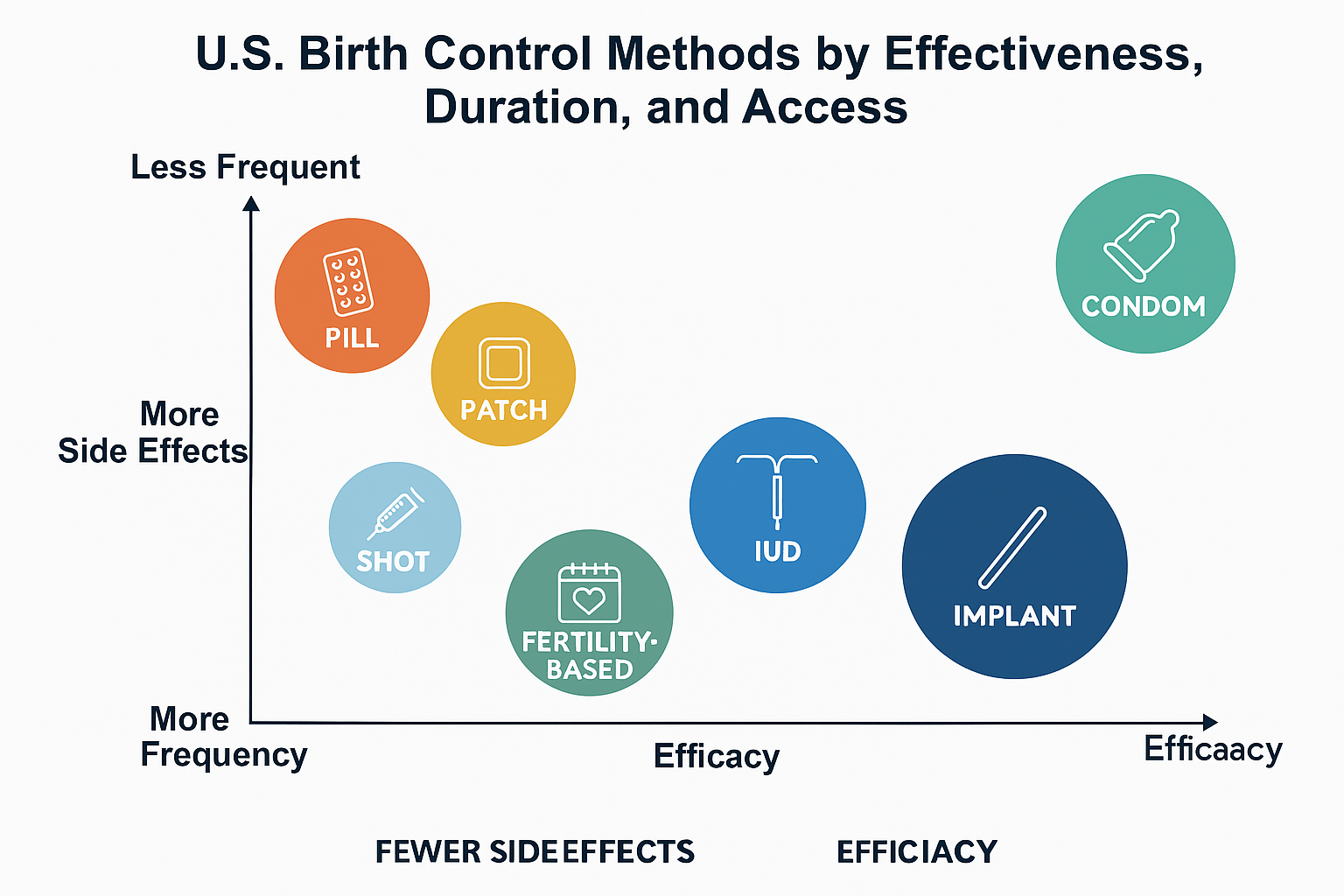
Birth Control Implant Overview
Birth control implant in arm (brand name: Nexplanon) is a thin, flexible rod inserted by a
healthcare provider under the skin of the upper arm.
How it works
Releases progestin slowly to suppress ovulation and thicken cervical mucus.
Effectiveness: Implant is over 99% effective, making it one of the most reliable methods
available.
Duration: Protects against pregnancy for up to 3–5 years.
Side Effects: Irregular bleeding or spotting is the most common side effect; some may
experience headaches, weight gain, or mood changes. Most side effects decrease over time.
Insertion/Removal: Quick outpatient procedure; fertility returns quickly after removal.
Birth Control Shot
The Depo-Provera shot is a progestin injection given every 12–13 weeks.
How it works: Stops ovulation, thickens cervical mucus.
Effectiveness: With perfect use, 99%; with typical use, around 94%.
Notable side effects:
● Irregular bleeding, especially at first
● Weight gain can be more pronounced compared to other methods
● Some women experience a temporary decrease in bone density, hence long-term use is
generally limited to 2 years
● Fertility may take up to a year to return after stopping
Birth Control Patch
There are two main hormone patches on the U.S. market: Xulane and Twirla.
How it works:
Both are combination estrogen/progestin, releasing hormones transdermally
(through the skin). Worn on the stomach, buttocks, or upper body and changed weekly for three
weeks, followed by a patch-free week.
Effectiveness: With perfect use, over 99%; typical use is about 91%–93%.
Differences:
● Xulane releases a slightly higher estrogen dose than Twirla, and Twirla is not approved
for women with a BMI ≥30 due to reduced efficacy and increased risk of blood clots.
● Both have similar side effect profiles to pills: irritation at the patch site, headaches,
nausea, and breast tenderness. Some women experience lighter or absent periods.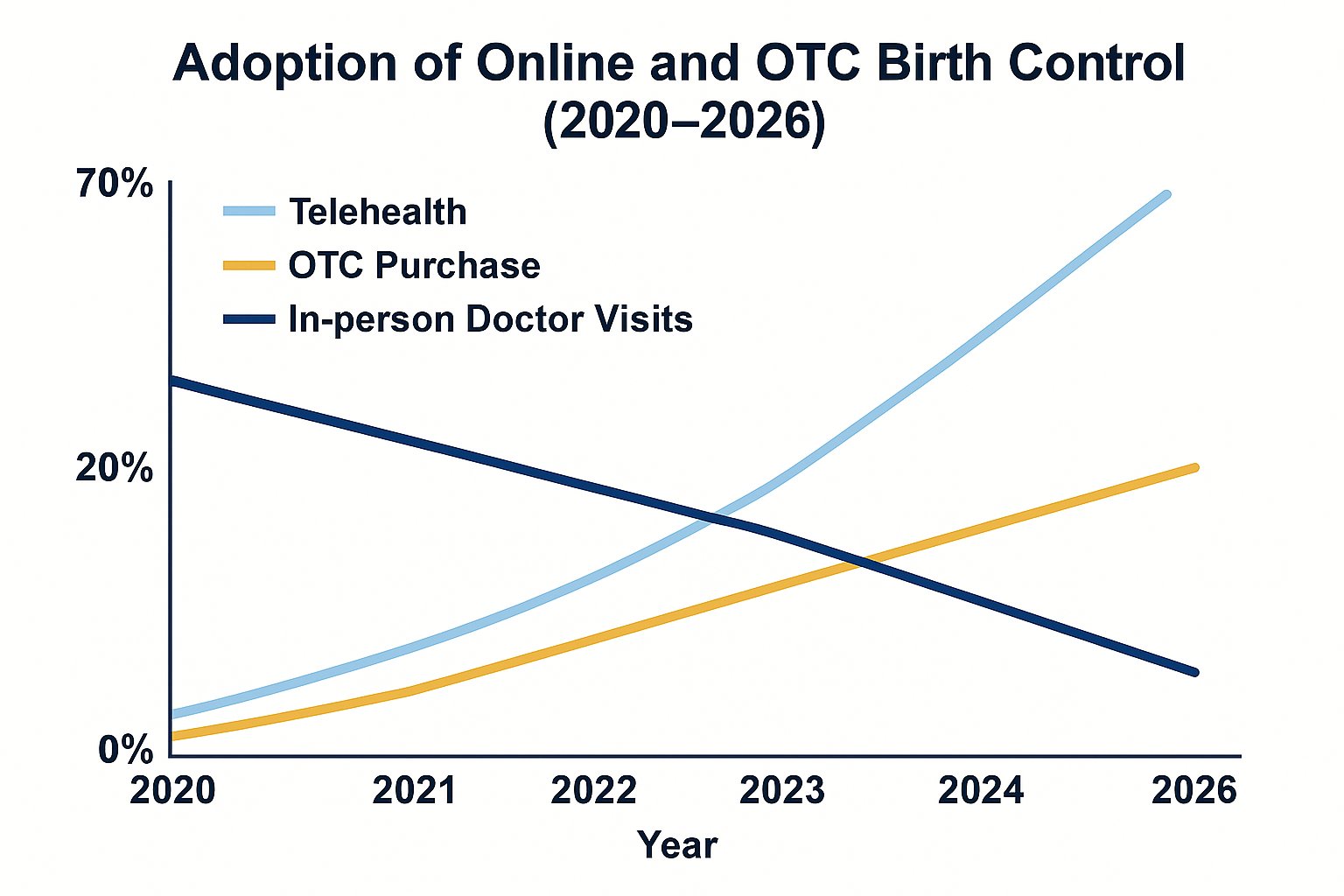
Birth Control Online: The Telehealth Wave
Getting birth control online has surged since 2020. Telehealth providers (e.g., Nurx, Pandia
Health, Wisp, Planned Parenthood Telehealth) offer virtual visits, prescriptions, and delivery of
birth control, often with consultation fees ranging from $0–$30. Most forms, especially pills,
rings, and patches, can be obtained this way.
Key statistics:
● The majority use online services for convenience; the most popular methods are pills
and patches.
● Insurance often covers medications fully, but prescription and consultation fees may still
apply.
Risks: Users should be aware that telehealth doesn’t replace regular gynecological care;
in-person screening for contraindications or other health issues remains essential.
Comparison Table of Common Birth Control Methods
.
| Method | Efficiency | Schedule | Side effects | STI Protection |
| Combination pill | (91-93)% | Daily,Same Time | Nausea,Headache,Mode changes | No |
| Progesting-Only pill | (91)% | Daily,Strict timing | Supporting,Breast tenderness | No |
| Birth control Implant | (99+)% | Inserted,Lasts(3-5) Years | Irregular Bleeding, Mood Swings | No |
| Condon (Male/Female) | (79-87)% | Every Act,As Needed | Allergy,Irritation | Yes |
Birth Control Pills: More Details :How They Work & Types
Birth control pills primarily prevent ovulation. All brands fall under two main categories:
● Monophasic: Same hormone dose daily (e.g., Sprintec, Junel, Yaz)
● Multiphasic: Doses vary to mimic the natural cycle (e.g., Ortho Tri-Cyclen)
● Extended-cycle/Continuous: Reduce frequency of periods (e.g., Seasonique, Amethia)
Progestin-only minipills (e.g., Slynd, Camila) are ideal for those who cannot take estrogen,
such as women over 35 who smoke or have a history of blood clots.
Side Effects & Risks
Most women tolerate pills well, but side effects—if present—usually resolve within a few
months:
● Mild: Spotting, nausea, breast tenderness, low mood
● Serious (rare): Blood clots, stroke, hypertension—risk increases with age and smoking;
certain progestins like drospirenone (as in Yasmin, Yaz) may increase clot risk.
Latest research also highlights some subtle impacts on mood and stress response, especially
when started during adolescence, although for most women, the benefits far outweigh these
concerns.
Non-contraceptive Benefits
Pills are FDA-approved to treat:
● Irregular or heavy periods
● PCOS
● Endometriosis
● Severe menstrual cramps
● Premenstrual dysphoric disorder (PMDD)
● Anemia from heavy bleeding
● Acne, hirsutism
Can a Woman Get Pregnant on Birth Control?
No method is 100% effective, but the risk of pregnancy on consistent pill use is very low (≈1–3%
per year with typical use; ≈0.3% with perfect use). Missing even a single pill or starting late
increases the risk, and certain medications or gastrointestinal issues (vomiting, severe diarrhea)
can interfere with absorption and efficacy.
Does Birth Control Stop Periods?
Many forms—including continuous-use pills, some hormonal IUDs, and the shot—can stop
menstrual periods or make them lighter and less frequent. Skipping placebos with combination
pills or continually switching to a new ring or patch is safe for most women and can reduce
painful or heavy bleeding. Progestin-only pills, however, require continuous daily use and do not
reliably stop menstruation.
Birth Control Implant: What to Expect
What Is the Birth Control Implant in Arm?
Nexplanon, the only birth control implant currently sold in the U.S., is inserted subdermally in the
upper arm by a trained provider.
Key advantages:
● Over 99% effective with a “set it and forget it” convenience
● Lasts up to 3–5 years
● Fertility returns rapidly after removal
● Especially beneficial for those who find daily or weekly contraception difficult
Side Effects:
● Irregular bleeding is the most frequently reported issue, but for some women periods
stop entirely
● Headaches, mood changes, acne, and weight gain are possible but not universal
● No estrogen, so safe for women with estrogen-related risks.
Insertion & Removal: The process is quick and done in-office; removal is equally swift. Any
birth control-related side effects resolve after removal, and women can get pregnant quickly if
desired.
Birth Control Patch: Painless, Weekly, and Clean
The patch offers an excellent alternative for women who don’t want to take a daily pill. Worn on
the skin and changed weekly, it delivers consistent hormone doses.
Xulane vs Twirla:
● Xulane: Higher estrogen content, more options for placement
● Twirla: Lower estrogen, round shape; not approved for women with BMI ≥30
Benefits:
● Easy to use; just remember the schedule (three weeks on, one week off)
● Can safely “stack” patches (no off-week) to skip periods, although more clinical studies
exist for continuous pills/rings
● Some women experience lighter, more regular, or no periods.
Risks:
● Similar to the combination pill (nausea, breast tenderness, headache, higher risk for
blood clots)
● Skin irritation or allergic reaction is possible
Access:
● Requires a prescription but available online via telemedicine with rapid shipping and
auto-refills.
Birth Control Shot: Powerful, Long-Lasting, but Unique Effects
The Depo-Provera shot is entirely progestin and requires a quarterly medical visit (or
self-injection at home where approved).
Pros:
● Highly effective; especially useful for women who cannot use estrogen
● Convenient — just four shots a year
● Can reduce menstrual cramps and cause periods to stop over time.
Cons:
● Can delay return of fertility for up to a year after the last shot
● Commonly causes weight gain, mood changes, and irregular bleeding
● Linked to temporary bone density loss, particularly in long-term users.
This method is especially appealing for those who struggle with daily/weekly regimens or don’t
want an implanted device.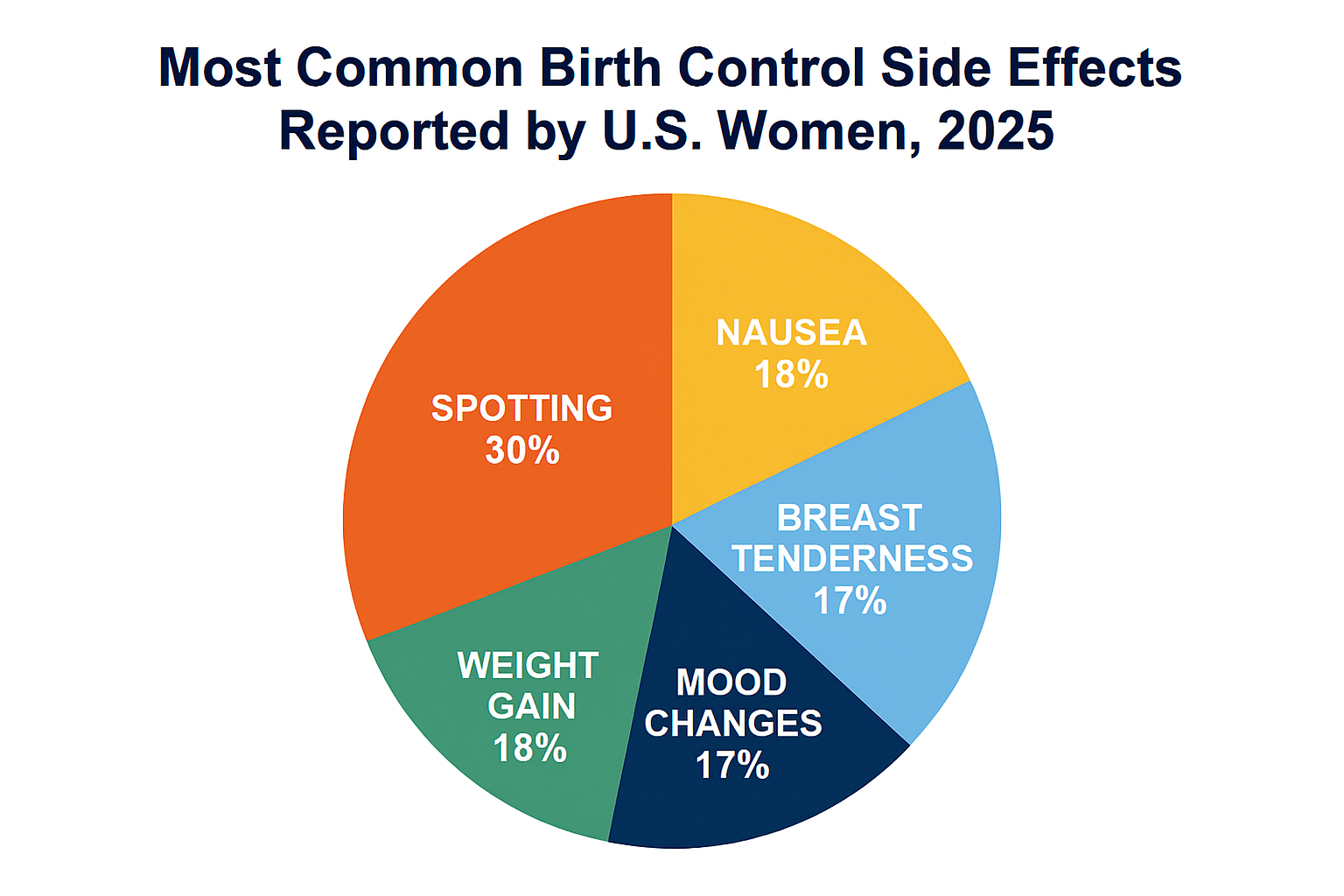
Side Effects of Birth Control: What Every Woman Should Know
General Birth Control Side Effects
● Hormonal methods (pills, patch, shot, implant): Common side effects include irregular
periods (spotting or missed), nausea, breast tenderness, mood changes, slight weight
fluctuations, and in rare cases, clotting events or hypertension.
● Non-hormonal methods: Copper IUDs may cause heavier periods and cramps; typical
barrier methods (condoms, diaphragm) may cause irritation or allergies.
● Emotional & cognitive: Recent research suggests hormonal contraceptives can affect
stress responses, mood, and, for a small subset, even cognition, but for most women,
the benefits remain significant. Notably, starting hormonal birth control in adolescence
may slightly increase depression risk later in life.
Most side effects diminish with continued use or by switching brands/types. Always consult your
provider to find the best fit for you.
Birth Control and Weight Gain
Most modern birth control pills do not cause significant weight gain; any changes are typically
related to fluid retention. The birth control shot (Depo-Provera) and implant are more likely to be
associated with weight gain.
Birth Control and Cancer/Fertility
● Combined hormonal methods may slightly increase the risk of breast and, for longer
use, cervical cancer but lower the risk of endometrial and ovarian cancers.
● Fertility returns quickly after stopping most birth control, except after the shot, which can
delay fertility for up to a year. Birth control does not cause long-term infertility.
“Can I Get Pregnant on Birth Control?” and Other Key Questions
● Perfect use is nearly 100% effective, but missed pills or late patches dramatically
reduce efficacy. Some medications (antiepileptics, certain antibiotics, herbal
supplements like St. John’s Wort) reduce absorption.
● Pregnancy symptoms while on birth control should always prompt a pregnancy test.
“Does Birth Control Stop Periods?”
● Many women enjoy lighter, more regular, or even absent periods with hormonal birth
control
● Skipping periods by continuous use is safe and often improves iron status and quality of
life
● Progestin-only pills and some LARCs are less likely to regulate or stop periods.
Trends & Innovations in Birth Control (2025–2026)
New Developments
The U.S. FDA has recently greenlit several innovative birth control products:
● Long-acting vaginal rings (Annovera) that can be reused for up to a year, needing no
refrigeration, and offering an alternative to daily pills.
● Progestin-only pills like Slynd, with improved safety for those who cannot tolerate
estrogen.
● Twirla patch, which has a lower estrogen dose and broadened patch options.
● Phexxi spermicide gel, a non-hormonal, pH modifying spermicide that is less irritating
to the vaginal lining
● Over-the-counter Opill, a progestin-only pill, now adds latest access for those wanting
contraception sans prescription.
● Next-generation copper IUD (MIUDELLA), now the smallest non-hormonal IUD
available in the U.S., with less copper, and fewer side effects. Research also continues
into male hormonal contraceptives, new adhesives for patches, and digital tracking and
counseling tools for personalization.
Policies & Access
● The Access to Birth Control Act (2025–2026) currently in Congress would further require
pharmacies to provide all FDA-approved contraceptives without delay or discrimination,
responding to ongoing barriers after the Dobbs v. Jackson decision. It also underscores
the fundamental right to contraception in the U.S.
● Anti-abortion and anti-contraception policies fluctuate at the state level, but federal
guidance continues to expand coverage and reduce cost-sharing through the ACA.
Online Birth Control Access
● Telehealth platforms (e.g., Nurx, Wisp, Pandia Health, Planned Parenthood) have made
pills, patches, and rings more accessible. Most services offer annual consultations for
$0–$30, insurance billing, and discreet home shipping.
Access to Birth Control in the U.S.: Cost, Coverage, and Legal Landscape
Insurance & Out-of-Pocket Costs
● ACA Coverage: Most employer-sponsored and ACA marketplace plans cover at least
one version per contraceptive method with no copay; generic birth control pills and
patches often cost $0 for those with insurance.
● Uninsured: The out-of-pocket cost for pills averages $20–$84/month; patches and rings
are $50–$200/month; IUDs and implants cost $1,000–$1,500 initially but are covered
when insurance is present or at public clinics.
● OTC Options: Opill now retails for about $340/year, competitive with generic
prescriptions.
Free and Low-Cost Programs:
● Planned Parenthood and community clinics offer free/reduced fees based on income.
● Medicaid and state-run family planning programs cover most methods for eligible
individuals.
Policy Challenges
● Despite increased coverage, barriers remain due to recent state-level restrictions,
provider refusal, and insurance gaps.
● The Access to Birth Control Act and HHS guidance have clarified the right to
contraception and reduced pharmacy refusals, but some states still restrict minor access
or specific contraceptives.
Myths and FAQs
● Is Plan B the same as the abortion pill?
No. Plan B (levonorgestrel) prevents or delays ovulation and cannot terminate an
established pregnancy.
● Are cycle-tracking apps a replacement for birth control?
Not advisable: Fertility awareness methods have higher typical-use failure rates and
relying solely on apps can lead to unintended pregnancies, especially in states with
harsh abortion laws.
● Does emergency contraception cause abortion?
No. Emergency contraceptive pills work before implantation and do not harm an existing
pregnancy.
● Will I lose fertility after stopping birth control?
No. Most women return to their baseline fertility within weeks to months (except for the
shot, which can take longer).
● Can birth control delay or skip periods safely?
Yes, using continuous pills, the patch, or the ring to skip periods is both safe and
common.
How to Choose the Best Birth Control Method for You
● Consider your health history (blood clots, migraines, cancer risk)
● Decide on desired frequency: daily, weekly, monthly, or long-acting “set and forget”
● Think about side effect tolerance (e.g., mood, bleeding, weight)
● Evaluate convenience and privacy (e.g., online order vs. clinic visit)
● Factor in non-contraceptive benefits (e.g., acne, regulated periods)
● Don’t forget STI protection—only condoms offer this
● Check insurance or local program coverage for zero/low cost
● Discuss with a provider or use reputable online decision tools
Each point above can significantly affect satisfaction and long-term use, so personalizing your
choice is the best way to maximize benefits and minimize hassle.
Conclusion
Today’s birth control landscape in the United States, heading into 2025 and 2026, offers
unprecedented options, convenience, and personalization for women—yet remains shaped by
personal, political, and practical realities.
Understanding the basics of what birth control means,
how different methods work, and their real-world pros, cons, and risks is essential for making
empowered choices about reproductive health.
Whether you prefer daily birth control pills, a discreet implant in your arm, the low-maintenance
patch or shot, or want the flexibility of online ordering and telehealth visits, the good news is that
modern birth control is highly effective, accessible, and now even more affordable for most
women.
Still, no method is perfect for everyone: side effects, lifestyle fit, insurance barriers, and
state laws can all influence what is best for YOU.
As you explore your options, keep these key points in mind:
● Nearly all methods are covered by insurance, and most women can access free or
low-cost birth control methods.
● Side effects are manageable for most, with serious risks being rare.
● Online access is growing rapidly, but should not entirely replace routine in-person
gynecology visits.
● Don’t hesitate to try a new method if your current choice isn’t working for you, and
always consult a provider for personalized recommendations.
For optimal results—whether your goal is pregnancy prevention, better periods, or support for a
medical issue—stay proactive, seek out reputable information, and don’t be afraid to ask
questions.
Your health, your body, your birth control—make the choice that fits your life. And if
you’re ready to take the next step, reach out to your healthcare provider or visit a trusted online
provider today.
Ready to find your fit? Book an appointment with Planned Parenthood, or explore CDC’s
birth control resources for up-to-date, U.S.-specific guidance.
Your future, your decision. Take charge today!
Frequently Asked Questions (FAQ)
Q1: What is birth control, and how does it work?
Birth control, also known as contraception, refers to medications, devices, or procedures used
to prevent pregnancy. Methods range from hormonal (like pills, implant, patch, shot) that
suppress ovulation, to barrier methods that block sperm, to copper intrauterine devices (IUDs)
that create an inhospitable environment for sperm and eggs. Many options also thin the uterus
lining or thicken cervical mucus to prevent fertilization. Birth control is not only for pregnancy
prevention but also helps manage periods, treat menstrual disorders, and reduce the risk of
certain cancers.
Q2: What are birth control pills, and what side effects should I expect?
Birth control pills are daily oral contraceptives containing estrogen, progestin, or both. They’re
91–99% effective depending on use, and come in multiple brand and generic options (e.g.,
Sprintec, Yasmin, Junel, Slynd).
Common side effects: nausea, headaches, breast tenderness, mood changes, and
occasional spotting or missed periods, most of which subside in a few months.
Serious risks (rare): blood clots, stroke, or high blood pressure, mainly in smokers over 35.
Benefits include lighter, more regular periods, less acne, and reduced risk of endometrial and
ovarian cancer.
Q3: Can a woman get pregnant on birth control?
While no contraceptive is 100% effective, proper use of most modern methods results in less
than a 1–3% annual pregnancy rate. Missing pills, delays in patch or shot, or certain
medications can elevate the risk. If you miss multiple pills or have symptoms of pregnancy, use
emergency contraception and consult your provider.
Q4: Does birth control stop periods, and is it safe to skip them?
Yes, many hormonal methods (continuous-use pills, some IUDs, the shot, or stacking
patches/rings) can stop or reduce periods. This is safe for most women and often beneficial for
those with heavy, painful, or inconvenient periods. Consult your doctor if you skip periods for
unknown reasons, have new symptoms, or want to start a continuous regimen.
Q5: How do I access birth control online, and is it as safe as seeing a doctor in person?
Online birth control is available via telehealth platforms (e.g., Nurx, Pandia Health, Planned
Parenthood), offering a virtual consultation and direct shipment to your home. These services
are convenient, private, and usually covered by insurance.
However, they do not replace routine in-person exams for health checks, Pap smears, or STI screening.For ongoing safety, keep up with regular gynecology visits.
Q6: How much does birth control cost in the U.S.?
With insurance (especially under the ACA), most contraceptives (pills, patch, ring, IUD, implant)
are free or low-cost. Out-of-pocket, pills run $20–$84/month, patch/ring up to $200/month, shot
about $150 each, and LARC methods can cost up to $1,500 up front without insurance—but
programs like Planned Parenthood often reduce these costs to $0–$50. OTC Opill costs about
$340/year for a progestin-only option you can get without a prescription.
For help, book an online consult with Planned Parenthood or find low-cost resources.

